Table of Contents
- Upper Endoscopies Help Combat Celiac Disease
- Endoscopy and Biopsy: The Gold Standard for Diagnosing Celiac Disease
- Diagnosing Other GI Issues with Upper Endoscopies
- ColonoscopyAssist: Diagnosing Celiac Disease without Breaking the Bank
- Conclusion
- FAQs
When it comes to understanding and diagnosing digestive issues, sometimes you need more than just symptoms or a blood test. That’s where esophageal endoscopy (EGD) steps in. This procedure provides a clear, detailed look inside the digestive tract and can collect tissue samples that offer definitive answers for conditions like celiac disease, GERD, and ulcers.
Let’s explore why EGD is such a valuable tool in diagnosing and managing gastrointestinal problems and how it helps catch issues early, paving the way for effective treatment.
Approximately 1.4% of the global population tests positive for celiac disease–specific antibodies, indicating potential celiac disease. However, the prevalence confirmed through biopsy is about 0.7%.
How EGD Helps Combat Celiac Disease
Blood tests for celiac disease (antibody screenings) are a good start. But they can’t confirm the diagnosis of celiac disease. Gastroscopy with biopsy is the gold standard for diagnosis, as it allows direct visualization of the small intestine and tissue samples to be taken. These biopsies are examined for damage to the villi in the duodenum, the tiny finger-like projections lining the small intestine that are responsible for nutrient absorption. Flattened or damaged villi are the hallmark of celiac disease.
EGD also helps to rule out other conditions that have similar symptoms like irritable bowel syndrome (IBS). This is important for proper treatment like confirming the need for a lifelong gluten-free diet. Without accurate diagnosis symptoms may persist or worsen due to untreated intestinal damage.
Also gastroscopy is useful for monitoring celiac disease. If symptoms persist despite being on a gluten-free diet, follow up esophageal endoscopy can evaluate healing and rule out complications or other underlying issues.
Diagnosing Celiac Disease with Biopsies and Upper Endoscopies
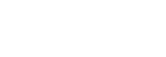
The Biopsy can show the following signs in the small intestine:
- Increased White Blood Cells: There may be a higher number of certain immune cells (white blood cells) called intra-epithelial lymphocytes (IELs) in the intestine lining.
- Longer Grooves Between Villi: The grooves between the small fingerlike structures (called villi) in the intestine may be longer than normal. This is called crypt hyperplasia.
- Shrunken or Flattened Villi: The villi, which help absorb nutrients, might shrink or flatten. This often happens after repeated exposure to gluten in people with celiac disease.
- Extra Immune Cells in Tissue Layers: There may be an increase in immune cells in the layer of tissue under the intestine’s surface, called the lamina propria. This tissue works as a protective barrier to keep harmful substances out.
- Changes in the Lining of the Intestine: The cells that make up the intestine lining might show changes in their structure, indicating damage or abnormal growth.
During the endoscopy, the doctor can see changes in the small intestine, such as folds that look flattened or uneven, grooves or cracks on the folds, and a surface that appears patchy or has a pattern like a mosaic.
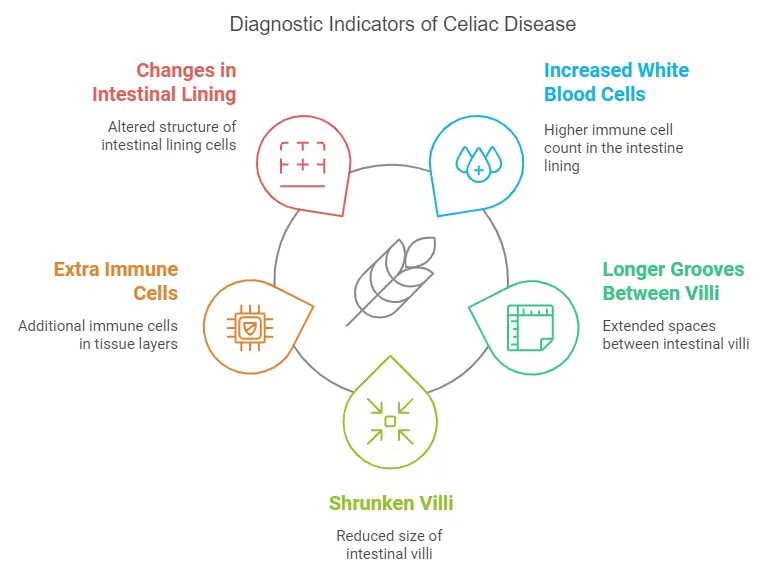
Additionally, an EGD is preferred for several reasons:
Biopsy Accuracy
The ability to take tissue samples during gastroscopy is key to diagnosing conditions like celiac disease, ulcers and Barrett’s esophagus. Biopsies give you the answers that blood tests and imaging can’t.
Subtle Changes
Upper GI endoscopy can detect microscopic changes in the lining of the stomach tract like early villous atrophy in celiac disease or mild esophagitis in GERD. These subtle findings are often missed by other methods.
Early Intervention
Early detection is key in gastroenterology for managing autoimmune conditions. Diagnosing conditions like celiac disease, GERD or Barrett’s esophagus early will allow for timely treatment and prevent long term complications like malnutrition, esophageal cancer or severe ulcerations.
Comprehensive Evaluation
EGD provides a direct view of the esophagus, stomach, and upper small intestine. This comprehensive evaluation allows physicians to assess the overall health of the gastrointestinal lining and identify coexisting issues, such as inflammation, polyps, or infections, that might not present clear symptoms initially.
Monitoring Progression
For patients with chronic conditions like celiac disease or GERD, EGD is an excellent tool for monitoring disease progression or assessing the effectiveness of treatment. For instance, follow-up EGDs can confirm whether dietary changes in celiac disease are restoring the intestinal lining or whether GERD management strategies are preventing further esophageal damage.
Personalized Care
The real-time visualization during an EGD helps gastroenterologists tailor treatment plans to the unique needs of each patient. For instance, seeing the exact extent of villous atrophy in celiac disease can influence dietary recommendations and follow-up care.
Diagnosing Other GI Issues with Upper Endoscopies
An Upper endoscopy is useful for many GI disorders beyond celiac disease. Here’s how it helps in specific cases:
GERD and Barrett’s Esophagus
For those with chronic acid reflux (GERD), esophageal endoscopy evaluates the esophagus and rules out complications like Barrett’s esophagus, which can be related to gluten intolerance. This is a condition where the lining of the esophagus changes and can increase the risk of esophageal cancer. Early detection through EGD can prevent long term complications.
Ulcers and Gastritis
Gastroscopy is also used to diagnose ulcers caused by Helicobacter pylori infections or prolonged use of nonsteroidal anti-inflammatory drugs (NSAIDs). By visualizing the ulcers and taking biopsies, this procedure will identify the underlying cause and guide treatment to prevent bleeding or perforation.
Structural Issues and Tumors
Structural abnormalities like strictures (narrowing of the digestive tract), polyps, or tumors can cause unexplained symptoms and may be related to undiagnosed conditions. EGD will give you a direct view of these issues and allows immediate biopsies for prompt diagnosis and management.
Food-Related Disorders
Eosinophilic esophagitis (EoE) an allergic inflammatory disorder of the esophagus can also be evaluated with gastroscopy. This condition often mimics GERD but biopsies taken during the procedure will reveal eosinophils, a type of white blood cell associated with allergic reactions.
ColonoscopyAssist: Diagnosing Celiac Disease without Breaking the Bank
If you have persistent symptoms, ColonoscopyAssist offers low cost colonoscopy services. Our team will give you the clarity to make informed decisions about your health.
Don’t wait—schedule your EGD today and start your journey to better digestive health.
Final Thoughts
Upper endoscopy is the base of GI diagnostics. It’s the most accurate way to diagnose celiac disease, GERD, ulcers and structural issues. With early and precise diagnosis this procedure will help you plan better and have better outcomes. If you suspect celiac disease or have persistent symptoms related to gluten, talk to your doctor or schedule an EGD. Early detection is important.
FAQs
How does a gastroenterologist check for potential celiac disease?
A gastroenterologist typically begins by evaluating your symptoms and medical history. The initial step often includes blood tests to check for specific antibodies, such as tissue transglutaminase antibodies (tTG-IgA) and deamidated gliadin peptide (DGP) antibodies, which can indicate an immune response to gluten. If these tests suggest celiac disease, the next step usually involves an upper endoscopy with a biopsy of the small intestine to confirm the diagnosis. During this procedure, a small camera is used to examine the small intestine, and tissue samples are collected to check for signs of damage caused by gluten.
What confirms the diagnosis of celiac disease?
A definitive diagnosis of celiac disease is confirmed through a combination of blood tests and a biopsy of the small intestine. Positive blood tests for celiac-specific antibodies (like tTG-IgA) suggest the condition, but the gold standard is an intestinal biopsy obtained during an upper endoscopy. The biopsy allows the gastroenterologist to examine the tissue for villous atrophy, crypt hyperplasia, and other signs of gluten-induced damage. For some patients, genetic testing for HLA-DQ2 and HLA-DQ8 genes may be done to rule out the possibility of celiac disease if the genetic markers are absent.
What is the best test to diagnose celiac disease?
The best test to diagnose celiac disease is a combination of serologic testing and an intestinal biopsy. Blood tests for tTG-IgA and DGP antibodies are highly sensitive and specific for detecting celiac disease and its autoimmune response. If the blood tests are positive, an upper endoscopy with a small intestine biopsy is conducted to confirm the diagnosis. It is crucial to be on a gluten-containing diet before these tests, as eliminating gluten can affect the accuracy of the results.
How often should you get an endoscopy if you have celiac disease?
After the initial diagnosis of celiac disease, follow-up endoscopies are not routinely required for all patients. However, a gastroenterologist may recommend a repeat endoscopy if symptoms persist despite adherence to a strict gluten-free diet or if there are concerns about complications such as refractory celiac disease. In general, the need for subsequent endoscopies depends on individual circumstances, including symptom resolution, dietary compliance, and any new health concerns.
What is the role of capsule endoscopy in celiac disease?
Capsule endoscopy is a diagnostic tool that uses a small, pill-sized camera to capture images of the gastrointestinal tract. While it is not typically the first-line test for celiac disease, it may be used in specific situations, such as when symptoms persist despite a gluten-free diet or if there are concerns about complications like small bowel strictures or refractory celiac disease. Capsule endoscopy can help detect abnormalities in areas of the small intestine that are not easily reached by standard endoscopy.