Table of Contents
As a patient, are you nervous about undergoing an EGD? If you are, that’s OK … you are not alone. A study estimated that 60-92% of patients feel some degree of anxiety prior to either surgery or an invasive medical procedure like an EGD, particularly concerning the possibility of complications such as bleeding. Anxiety is natural.
By helping you understand what to expect during the day of the procedure, you will understand the steps involved and the reasons behind each of the steps. By knowing more, much of your anxiety should fade away.
Arrival and Check-In
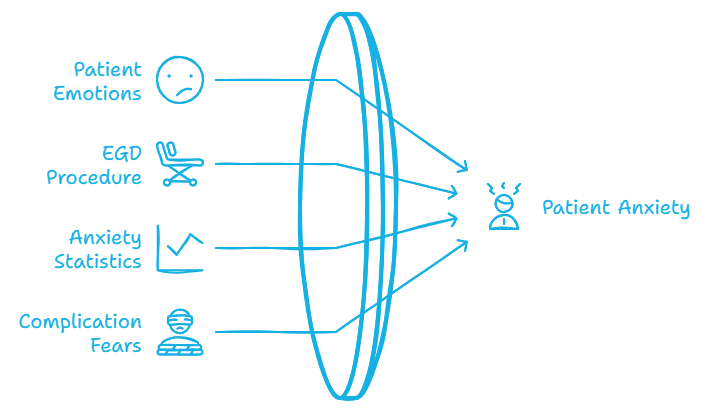
Regardless of the procedure, the check-in process for a medical procedure is nearly universal. It begins prior to the day of the procedure with pre-registration. When the EGD was scheduled, the patient would have answered questions about their medical history, and would have received instructions about fasting, any adjustments to current medications, and verifying insurance or self-pay information. Preparing well is key in having a successful endoscopy.
When the patient arrives at the medical facility, they will re-confirm much of the information they went over during pre-registration and provide proof of identity. The medical staff will verify that the patient followed the instructions from pre-registration, give an update as to what to expect during the day, and see what questions that the patient may still have. They will have you sign consent forms allowing the procedures to move forward. Because an EGD involves anesthesia, the patient will need to have a responsible adult with them to ensure they can safely return home after the procedure. The patient undergoing the endoscopy is being closely monitored for any signs of bleeding. They will not be allowed behind the wheel due to effects of sedation, nor will they be allowed to travel home unaccompanied.
Endoscopy Pre-Procedure Preparation
The patient will be escorted to a pre-operation area, where medical vitals will be taken, and the medical history and other patient information will be re-confirmed. The patient will put on a hospital gown and any personal belongings with them will be put into safe storage.
The medical staff will re-verify many of the questions asked previously to ensure no errors occur, especially regarding the patient’s history of gastroesophageal reflux disease. Before being taken to the operating room, an IV may be started to administer sedation or fluids, and monitoring devices may be attached to track blood pressure and oxygen levels.
The Procedure
The patient will be sedated to ensure their comfort. Most endoscopy patients receive conscious (moderate) sedation. In this process, you will be drowsy, unlikely to remember the procedure, but breathing on your own; you will also be advised not to eat or drink beforehand. Some patients may warrant a deep sedation, in which they are put completely to sleep during the procedure and need to have their breathing monitored.
The patient is usually laying on their left side with their head tilted slightly forward. This is done to provide the most optimal, low-risk path for the doctor to maneuver the endoscope. The gastric endoscope, a flexible tube, can vary in length, but typically is 3 to 5 feet.
Once the patient is sedated, the doctor will guide the endoscope through the mouth and down the esophagus into the stomach and upper portion of the small intestine. The bright light allows the doctor a clear visual inspection of the upper GI tract. The endoscope also allows the doctor to take tissue samples so that biopsies can be made, which is crucial for detecting any abnormal growths that could lead to bleeding. An EGD usually takes no more than 30 minutes to complete.
Upper GI Endoscopy Post-Procedure
Once the endoscopy is completed, the patient is moved to a recovery area. Nurses will observe the patient while the sedative wears off and will ensure that no problems arise after the procedure, as well as determine how they are feeling. Some potential side effects include:
- Drowsiness, dizziness, fatigue, (and in some extreme cases) nausea and vomiting due to the anesthesia.
- Sore throat from the endoscope passing through the esophagus.
- Bloating or gas from air being introduced during the procedure.
- Mild cramping
These issues are normal and short-term. Although the effects of sedation can vary, most patients can expect to go home within several hours after the procedure, provided there are no complications such as bleeding. The standard instructions involve relaxing the rest of the day, staying hydrated, and taking over-the-counter medicines for any lingering discomfort.
ColonoscopyAssist: Championing Lifesaving Procedures
ColonoscopyAssist is dedicated to making colonoscopies and other gastrointestinal procedures accessible and affordable for those without insurance or who are self-paying. Our program supports those committed to digestive wellness and colon health by offering affordable screening options.
Final Thoughts
By understanding what to expect on the day of your upper endoscopy, you’ll be well-prepared. Understanding all the steps in the process will remove much of the anxiety that is normal during a medical procedure. The procedure is quick, safe and minimally invasive. An EGD is an important tool in diagnosing issues and helping a patient maintain their digestive health, particularly in cases of gastroesophageal reflux disease.
FAQ
Do they put you to sleep for an upper endoscopy?
Yes, you will typically receive sedation for an upper endoscopy to ensure your comfort during the procedure. While you may not be completely unconscious, the sedation provided is strong enough to make you feel very relaxed or drowsy, and many patients don’t remember the procedure afterward. According to the National Institute of Diabetes and Digestive and Kidney Diseases, sedation is a standard part of this process.
How do they sedate you for an upper endoscopy?
The sedation is usually administered through an intravenous (IV) line placed in your arm. This allows the doctor to give medication that relaxes you and minimizes discomfort. Some clinics may also use a numbing spray to help ease difficulty swallowing the endoscope. The goal is to make the procedure as smooth and painless as possible while the doctor examines your esophagus, stomach, and duodenum.
Do you gag during an endoscopy?
To prevent gagging, a mouth guard is placed to keep your mouth open and protect the endoscope. While the sensation of the scope entering your throat may cause some discomfort, the sedation helps reduce your gag reflex significantly. If you have a mild sore throat afterward, it’s normal and typically resolves within a day.
What happens if I drink water before an endoscopy?
You may be asked to avoid drinking or eating anything for 8 hours before the procedure to ensure an empty stomach. If you accidentally drink water, it can increase the risk of complications, such as aspiration or perforation during the procedure. It’s essential to follow your doctor’s instructions closely, as failing to do so could lead to rescheduling the procedure. The Institute of Diabetes and Digestive and Kidney Diseases emphasizes that preparation is critical for safety and accuracy, especially for diagnosing conditions like GERD, heartburn, or unexplained symptoms.
What are the side effects of an endoscopy?
Most patients experience minimal side effects after an upper endoscopy, but some may notice a mild sore throat, temporary bloating, or a sensation of difficulty swallowing. Rarely, more serious complications like bleeding or perforation can occur, especially if the procedure involves taking tissue samples. Sedation can also lead to drowsiness or mild nausea, which typically resolves within a few hours. The National Institute of Diabetes and Digestive and Kidney Diseases highlights that these side effects are generally mild and manageable, with serious complications being uncommon. Always follow your doctor’s post-procedure care instructions to ensure a smooth recovery.